Introduction
Effective management of clinical waste in healthcare facilities is not merely a regulatory requirement; it is a vital aspect of public health and safety. Approximately 15% of healthcare refuse presents hazardous risks, making it crucial to understand the categories and proper disposal methods of clinical waste. This understanding is essential for mitigating health threats and protecting the environment.
Healthcare providers face numerous challenges in ensuring compliance and effective waste management. What strategies can they implement to navigate these complexities? This article explores the intricacies of clinical waste services, providing insights into effective strategies that can safeguard both patients and the broader community.
Define Clinical Waste and Its Categories
Clinical refuse refers to any waste generated during the diagnosis, treatment, or immunization of humans or animals. This type of refuse includes materials that can pose significant health and environmental risks if not managed appropriately. The primary categories of clinical waste are as follows:
-
Infectious Waste: This category encompasses materials that contain pathogens, such as blood-soaked items, cultures, and contaminated sharps. It is important to recognize that approximately 15% of healthcare refuse is classified as hazardous, with a substantial portion being infectious.
-
Hazardous Materials: These materials present dangers due to their chemical characteristics, including pharmaceuticals and other harmful substances. Effective management of hazardous materials is essential to prevent exposure to these harmful chemicals.
-
Radioactive Material: Generated from diagnostic and therapeutic procedures, this material contains radioactive substances and requires specialized handling and disposal methods to mitigate hazards.
-
General Refuse: This category includes non-hazardous materials that do not pose a risk, such as packaging and food waste, which typically accounts for about 85% of refuse generated in healthcare settings.
Establishing these classifications is crucial for efficient refuse segregation and removal, which are vital components of clinical waste services in healthcare environments. Implementing effective segregation practices within clinical waste services not only enhances safety but also ensures compliance with regulatory standards, ultimately safeguarding both public health and the environment.

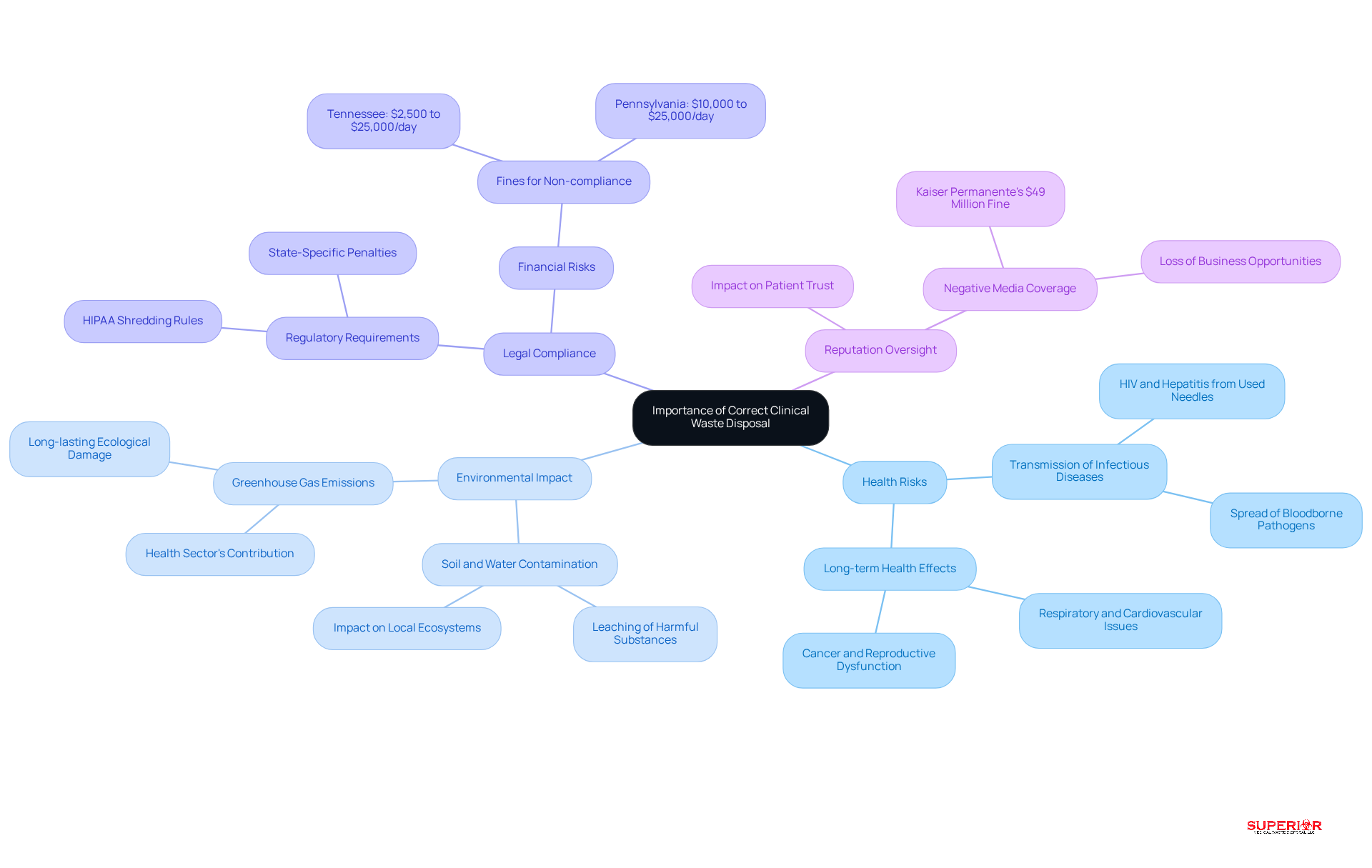
Understand the Importance of Correct Clinical Waste Disposal
Correct clinical waste disposal is essential for several reasons:
-
Health Risks: Inadequate management can facilitate the spread of infectious diseases, endangering healthcare workers, patients, and the broader community. For instance, used needles can transmit bloodborne pathogens such as HIV and Hepatitis, leading to severe health consequences.
-
Environmental Impact: Clinical refuse that is not disposed of correctly can leach harmful substances into soil and water sources, resulting in significant ecological damage. Research indicates that improper waste management practices can lead to long-lasting contamination, adversely affecting local ecosystems and agricultural productivity.
-
Legal Compliance: Healthcare facilities must adhere to stringent regulations governing refuse disposal, including HIPAA requirements for shredding protected health information (PHI) documents. For example, tax information should be retained for seven years before shredding, while customer contact information must be shredded within 30 days. Non-compliance can incur fines ranging from $2,500 to $25,000 per day in states like Tennessee and $10,000 to $25,000 per day in Pennsylvania, depending on the severity of the violation. This underscores the financial risks associated with improper disposal of materials.
-
Reputation Oversight: Facilities that neglect responsible refuse handling risk damaging their reputation, which can erode patient trust and disrupt business operations. High-profile cases, such as Kaiser Permanente’s $49 million fine for illegally disposing of private medical records and hazardous materials, illustrate the potential fallout from non-compliance.
By recognizing these implications, healthcare facilities can prioritize effective disposal management strategies that protect public health and the environment.
Implement Best Practices for Clinical Waste Disposal
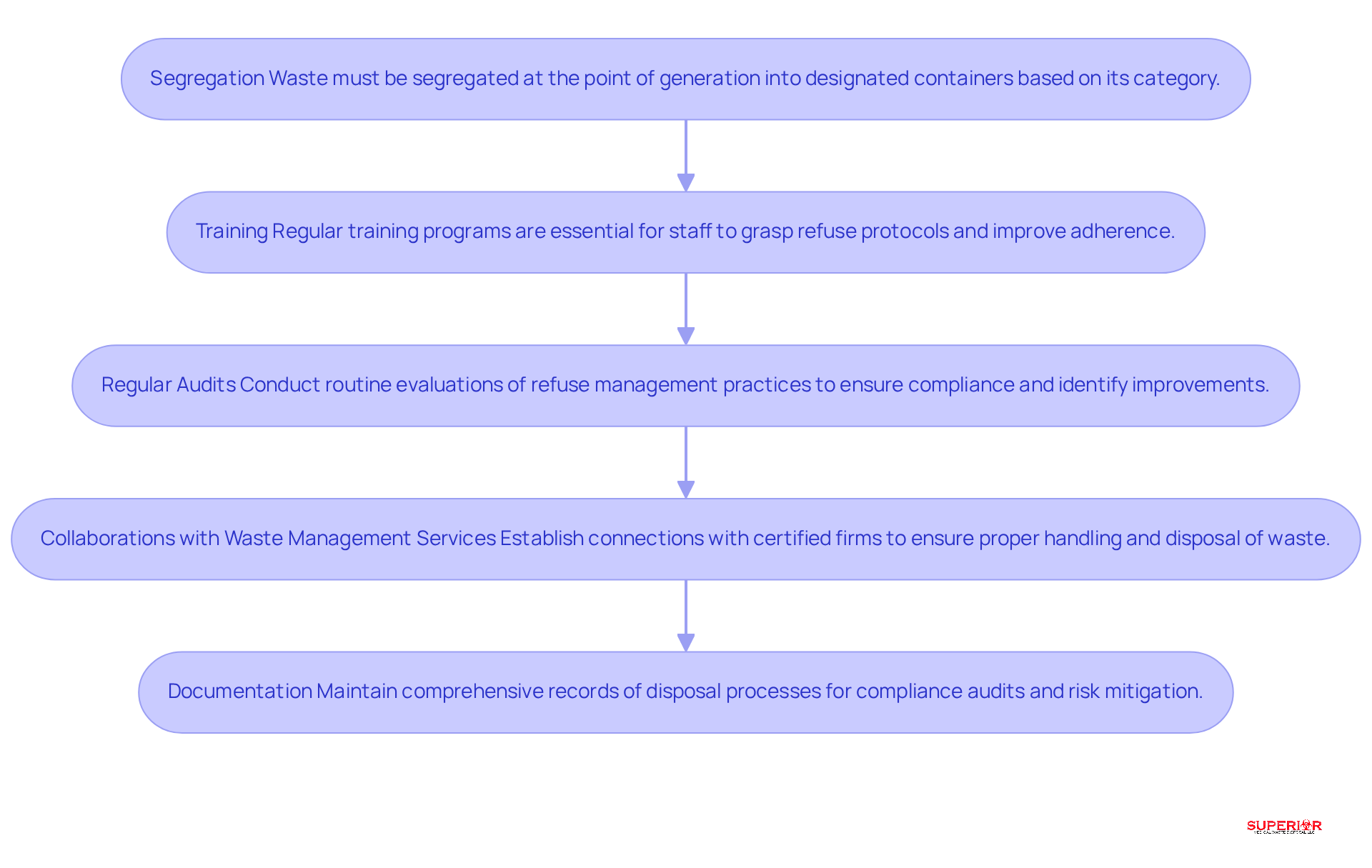
To effectively manage clinical waste, healthcare facilities should adopt several best practices:
-
Segregation: Waste must be segregated at the point of generation into designated containers based on its category. For instance, sharps should be discarded in puncture-resistant containers, while infectious materials need to be placed in biohazard bags. This practice not only mitigates risks but also facilitates proper disposal.
-
Training: Regular training programs are essential for staff to grasp refuse protocols, including proper segregation, handling, and disposal methods. Research indicates that effective training can lead to a 30% increase in adherence to segregation practices. Incorporating techniques such as quizzes and interactive sessions can enhance knowledge retention and foster a culture dedicated to resource conservation.
-
Regular Audits: Conducting routine evaluations of refuse management practices is crucial for identifying areas that require improvement and ensuring compliance with regulations. These audits can uncover gaps in knowledge and adherence, allowing for timely corrective actions.
-
Collaborations with Waste Management Services: Establishing connections with certified medical refuse management firms, such as Superior Medical Refuse Management, ensures that materials are handled and discarded in accordance with legal standards. It is important to consult local environmental authorities for guidance on regulations and handling procedures specific to your state. For example, in Michigan, biohazard materials must be removed by a licensed medical refuse hauler within 90 days. Collaborating with experienced partners can enhance operational efficiency and compliance.
-
Documentation: Maintaining comprehensive records of disposal processes, including quantities and types of materials disposed of, is vital for compliance audits. Accurate documentation demonstrates adherence to regulations and helps mitigate risks associated with improper disposal. In 2026, hospitals are projected to produce over 5 million tons of refuse annually, with 15% potentially infectious, underscoring the necessity for effective disposal practices. At Superior, our biohazard material is autoclaved and shredded to reduce volume by 70% before being sent to the landfill.
By implementing these best practices, healthcare facilities can significantly diminish the risks associated with clinical waste services, ensuring a safer environment for both staff and patients.
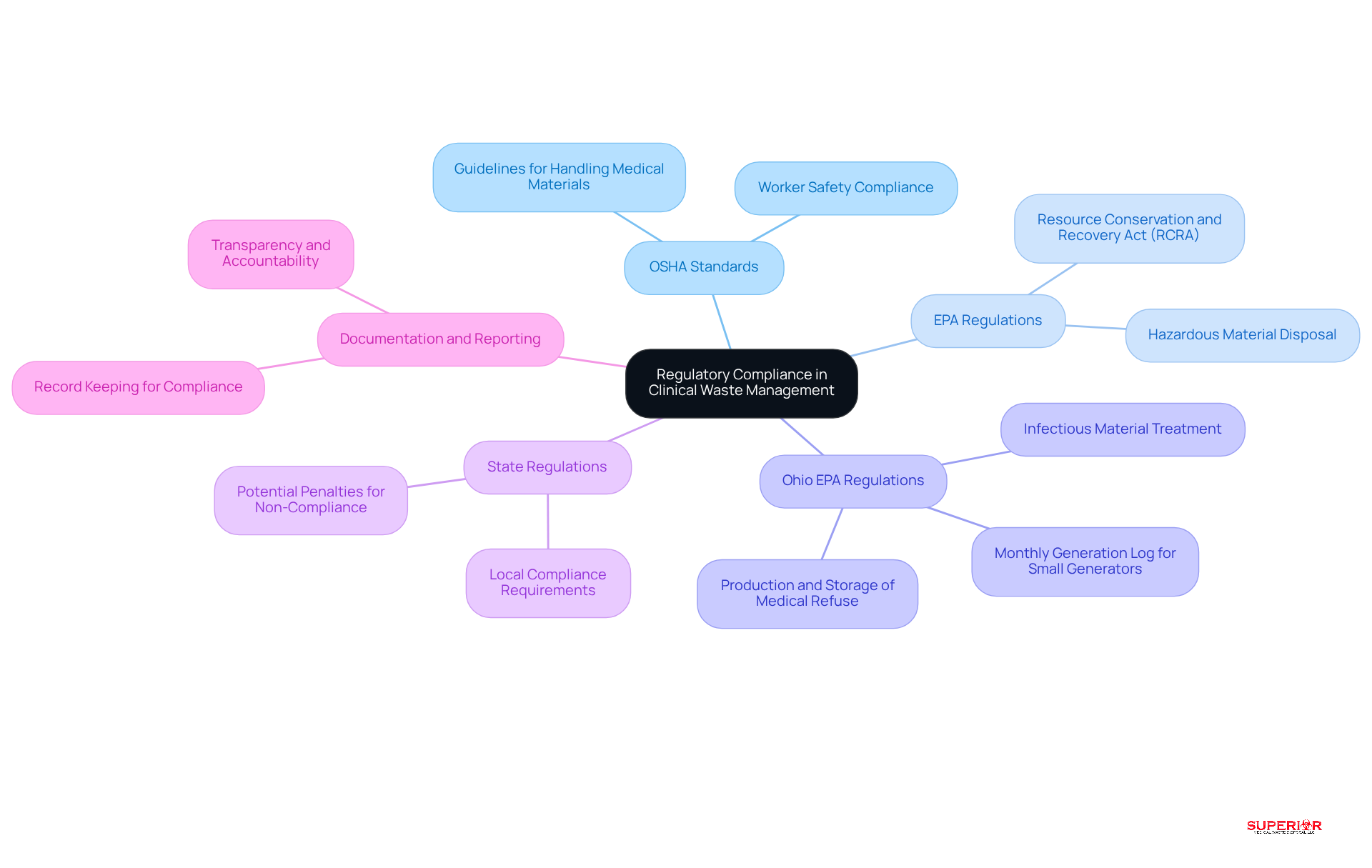
Navigate Regulatory Compliance in Clinical Waste Management
Healthcare facilities operate within a complex regulatory framework for clinical waste management, encompassing several critical regulations:
-
OSHA Standards: The Occupational Safety and Health Administration (OSHA) enforces guidelines governing the handling and removal of medical materials, ensuring the safety of healthcare workers. Compliance with these standards is essential to minimize exposure risks and maintain a safe working environment.
-
EPA Regulations: The Environmental Protection Agency (EPA) supervises the disposal of hazardous materials, including specific categories of medical refuse, under the Resource Conservation and Recovery Act (RCRA). This regulation mandates that hazardous medical materials must be treated or incinerated to neutralize pathogens and chemical hazards, thereby protecting public health and the environment.
-
Ohio EPA Regulations: In Ohio, the production, storage, and treatment of medical refuse are regulated by the Ohio EPA. While the medical disposal laws are more lenient than those in Michigan, compliance with these regulations remains crucial for healthcare facilities. The Ohio EPA advises that all infectious materials be dispatched to a commercial treatment facility, with autoclaving being the preferred treatment method. Small generators, producing less than 50 pounds of regulated medical refuse (RMW) per month, must maintain a monthly generation log of their infectious materials. Furthermore, it is essential to ensure the integrity of containers used for storage, and infectious materials must be stored in a manner that prevents them from becoming a food source or breeding ground for animals or insects.
-
State Regulations: In addition to federal guidelines, each state may enforce its own rules regarding medical refuse management. Healthcare facilities must remain informed about these local laws to ensure full compliance and avoid potential penalties.
-
Documentation and Reporting: Facilities are required to maintain comprehensive records of their refuse management practices. This documentation is vital for regulatory compliance and may be subject to review by regulatory bodies, ensuring transparency and accountability in disposal management practices.
By thoroughly understanding and adhering to these regulations, including those set forth by the Ohio EPA, healthcare facilities can effectively mitigate risks associated with clinical waste services, safeguarding their staff, patients, and the environment.
Conclusion
Effective management of clinical waste is crucial for healthcare facilities, as it significantly influences public health, environmental safety, and regulatory compliance. Understanding the various categories of clinical waste and implementing proper disposal practices allows healthcare providers to mitigate risks associated with infectious, hazardous, and radioactive materials. The importance of effective waste management extends beyond mere compliance; it cultivates a culture of safety and responsibility within healthcare environments.
Key insights emphasize the critical nature of:
- Waste segregation
- Staff training
- Regular audits
- Collaboration with certified waste management services
Each of these components is vital in ensuring that clinical waste is managed appropriately, thereby reducing potential health risks and environmental harm. Moreover, adherence to regulatory standards not only shields facilities from legal repercussions but also enhances their reputation among patients and the community.
Ultimately, the responsibility for effective clinical waste management rests with every member of the healthcare team. By prioritizing education and compliance, healthcare facilities can foster a safer environment for both patients and staff. Embracing these best practices is essential for protecting public health and preserving the environment, highlighting the necessity of a proactive approach to clinical waste disposal in the healthcare sector.
Frequently Asked Questions
What is clinical waste?
Clinical waste refers to any waste generated during the diagnosis, treatment, or immunization of humans or animals that can pose significant health and environmental risks if not managed appropriately.
What are the primary categories of clinical waste?
The primary categories of clinical waste are infectious waste, hazardous materials, radioactive material, and general refuse.
What is infectious waste?
Infectious waste includes materials that contain pathogens, such as blood-soaked items, cultures, and contaminated sharps. Approximately 15% of healthcare refuse is classified as hazardous, with a substantial portion being infectious.
What are hazardous materials in clinical waste?
Hazardous materials are those that present dangers due to their chemical characteristics, including pharmaceuticals and other harmful substances. Effective management of these materials is essential to prevent exposure to harmful chemicals.
What is radioactive material in the context of clinical waste?
Radioactive material is generated from diagnostic and therapeutic procedures and contains radioactive substances that require specialized handling and disposal methods to mitigate hazards.
What constitutes general refuse in healthcare settings?
General refuse includes non-hazardous materials that do not pose a risk, such as packaging and food waste, which typically accounts for about 85% of refuse generated in healthcare settings.
Why is it important to establish classifications for clinical waste?
Establishing classifications for clinical waste is crucial for efficient refuse segregation and removal, enhancing safety, ensuring compliance with regulatory standards, and ultimately safeguarding public health and the environment.
